This Article
Citations

Except where otherwise noted, this work is licensed under Creative Commons Attribution-NonCommercial 4.0 International License.
Hypoplastic Right Ventricle with Multiple Associated Anomaly: A Challenging Case for Biventricular Repair or Univentricular Approach?
Abstract
Abstract
Hypoplastic right ventricular is a rare congenital heart disease. A few cases have been reported. We presented a case with hypoplastic right ventricular and multiple associated anomaly (Ventricular septal defect, atrial septal defect and pulmonary stenosis) in whom the main concern was whether biventricular repair or Fontan type surgery would be the optimal management in this patient. Biventricular repair was done successfully using the multimodality cardiac imaging with intraoperative transesophageal echocardiography.
Keywords: Heart Ventricles; Right Ventricle Hypoplasia; Hypoplastic Left Heart Syndrome
1. Introduction
Hypoplastic right ventricle (RV) can be an integral part of malformations such as pulmonary atresia with intact ventricular septum and tricuspid atresia and occasionally is associated with a variety of congenital heart defects, such as ventricular septal defect (VSD), atrial septal defect (ASD), atrioventricular septal defet, and other complex congenital heart disease (CHD). A few cases with isolated hypoplastic RV and ASD have been reported (1-3). Surgical treatment of these patients is challenging. We reported a case with small RV for which the main question was proposed about the proper function of RV after ASD and VSD closure and whether RV would be able to function properly without increasing caval venous pressure.
2. Case Report
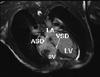
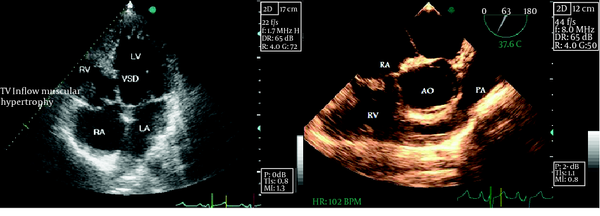
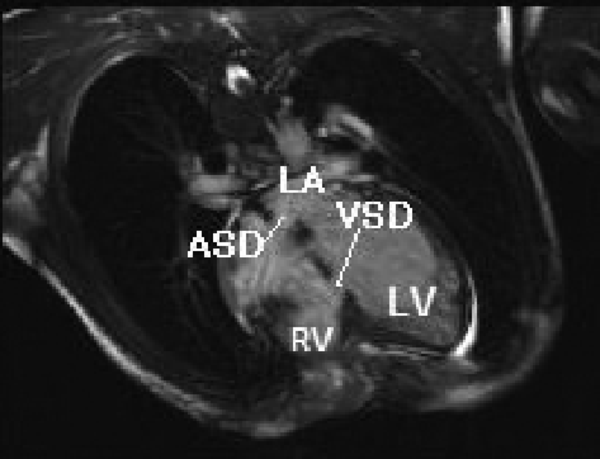
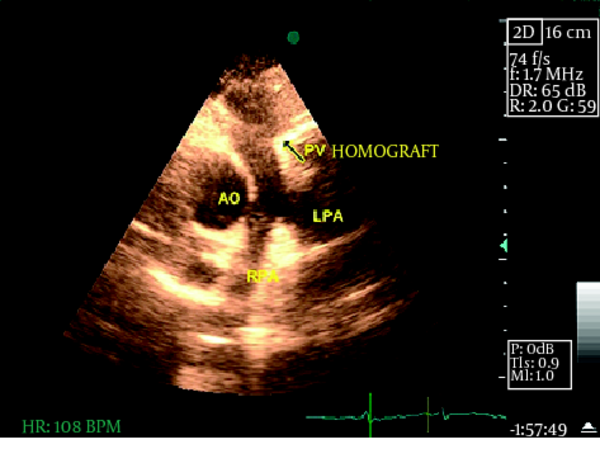
An 18-year-old man referred to our adult congenital heart disease (ACHD) clinic for Fontan type surgical treatment. He had cyanosis since infancy and exacerbation of dyspnea a few months ago. He had a history of palliative surgery (modified left BT shunt) when he was two years old with diagnosis of right ventricle hypoplasia, severe pulmonary stenosis, ASD and VSD with right to left shunt at both ventricular and atrial level, based on cardiac catheterization at that time. On physical examination, he had stable vital sign with severe cyanosis and clubbed fingers and toes. He was well nourished with body surface area about 1.6m 2 .The first heart sound was normal, the second one was soft. There was a grade 3/6 harsh systolic murmur at the upper left sternal border. Lab data showed secondary erythrocytosis (hemoglobin = 17g/dL). His chest x-ray showed normal cardiothoracic ratio with reduced pulmonary vascular marking and hypoperfused lung fields. Transthoracic echocardiography (TTE) and Transesophageal echocardiography (TEE) showed a moderate size secundum type ASD of 15 mm diameter with a right to left shunt and hypoplastic RV with small inlet (tricuspid annulus was 28 mm) and nearly absent outlet portion which was associated with subvalvular and valvular pulmonary stenosis and also moderate size mid muscular VSD (13 mm) with right to left shunt (Figure 1a-b). There was a persistent left SVC drain to coronary sinus and a poor functioning left BT shunt. Cardiac magnetic resonance (CMR) study was done for better evaluation of RV size and function. RV end-diastolic volume (RVEDV) was 52.25 ml and RVEDV index was 30.68 ml/m 2 , RV ejection fraction was 35%. The pulmonary valve annulus was 12 mm. Left ventricular end-diastolic volume (index) was 150.84 mL (88.58 ml/m2), and the left ventricular ejection fraction was 54% ; RV volume was about one third of LV volume (Figure 2); main pulmonary artery before bifurcation was 20 mm in diameter pulmonary artery branches (16mm in diameter each). We decided to candidate him for possible total biventricular repair. Patient underwent VSD closure with Gortex patch, partial closure of ASD, hypertrophied RV and infundibular muscles resection via tricuspid valve, and RV to pulmonary artery valved conduit (23-mm homograft) insertion, also previous shunt was sutured. Post pump intra operative transesophageal echocardiography (IOTEE) showed small residual ASD, small residual VSD, significant tricuspid regurgitation (TR), significant turbulence in right ventricular outflow tract (RVOT) with normally functioning pulmonary homograft. Regarding unstable hemodynamic with significant TR and RVOT stenosis, he underwent second pump run. Tricuspid valve was repaired and RVOT was enlarged by RVOT patch. Post pump IOTEE showed mild TR with no RVOT obstruction. He had uneventful early post operation follow up (Figure 3). His cyanosis was disappeared with 90% oxygen saturation by pulse oximetry at room air. He discharged in good condition and felt well at a 3-month follow-up visit.
|
Figure 1.
Echocardiographic Images
|
|
Figure 2.
Cardiac MRI Showing Small RV with ASD and VSD
|
|
Figure 3.
Post operation TTE showed normally functioning pulmonary homograft
|
3. Discussion
Hypoplastic RV is associated with malformed apical, inlet or outlet portion of the chamber. Our patient had small and hypertrophied inlet (tricuspid annulus 28 mm in diameter) and nearly absent outlet portion which was associated with subvalvular and valvular pulmonary stenosis. The main concern with this patient with regard to choosing the appropriate operative procedure was the right ventricular size and function. CMR is considered the best standard method for the evaluation of RV size and function. Variety numbers for normal range of RVEDV existed and we found the minimum range which was 58-154 ml and the RVEDV index was 57-95 ml/m2, vs. RVEDV 52.25 mL and index 30.68 ml/m2 of our patient. The patient could tolerate the surgery and RV obtained adequate size by RV inflow muscle resection and RVOT enlargement with patch augmentation. IOTEE had an important role for pre pump and post pump evaluations. Few cases with isolated RV hypoplasia and ASD have been reported and temporary occlusion of the ASD with a balloon catheter during preoperative study has been proposed to identify the patient suitable for simple closure of the ASD (1-5). In the present case, the balloon occlusion test was not conclusive, since the patient had multiple associated anomaly (ASD, VSD, PS). We considered the possibility of bidirectional Glenn anastomosis as a proper solution in the situation that small RV could not cope with the corrected situation and the superior caval venous pressure exceeds 20mmHg with low cardiac output immediately after coming off bypass surgery (6, 7). Noninvasive cardiac imaging was helpful in optimal management of this patient and he had successful repair and did fairly well on early follow up. Hypoplastic right ventricle with associated anomaly could be considered for biventricular repair by multimodality imaging support. A restrictive, residual ASD or VSD allows a controlled right-to-left shunt which may prevent excessive venous hypertension and allow adequate left-sided filling after biventricular repair.
Footnotes
References
- 1. Brown JW, Ruzmetov M, Minnich DJ, Vijay P, Edwards CA, Uhlig PN, et al. Surgical management of scimitar syndrome: an alternative approach. J Thorac Cardiovasc Surg. 2003;125(2):238-45. [PubMed]
- 2. Goh K, Sasajima T, Inaba M, Yamamoto H, Kawashima E, Kubo Y. Isolated right ventricular hypoplasia: intraoperative balloon occlusion test. Ann Thorac Surg. 1998;65(2):551-3. [PubMed]
- 3. Laks H, Pearl JM, Drinkwater DC, Jarmakani J, Isabel-Jones J, George BL, et al. Partial biventricular repair of pulmonary atresia with intact ventricular septum. Use of an adjustable atrial septal defect. Circulation. 1992;86(5 Suppl):II159-66. [PubMed]
- 4. Gatzoulis MA, Webb GD, Broberg CS, Hideki U. Cases in adult congenital heart disease. 1st ed. Churchill Livingstone Elsevier; 2009. 23 pp.
- 5. Van der Hauwaert LG, Michaelsson M. Isolated right ventricular hypoplasia. Circulation. 1971;44(3):466-74. [PubMed]
- 6. Kreutzer C, Mayorquim RC, Kreutzer GO, Conejeros W, Roman MI, Vazquez H, et al. Experience with one and a half ventricle repair. J Thorac Cardiovasc Surg. 1999;117(4):662-8. [PubMed]
- 7. Muster AJ, Zales VR, Ilbawi MN, Backer CL, Duffy CE, Mavroudis C. Biventricular repair of hypoplastic right ventricle assisted by pulsatile bidirectional cavopulmonary anastomosis. J Thorac Cardiovasc Surg. 1993;105(1):112-9. [PubMed]
 Home
Home Archive
Archive Search
Search Sign In
Sign In Site Menu
Site Menu Email this article to a friend
Email this article to a friend