This Article
Citations

Except where otherwise noted, this work is licensed under Creative Commons Attribution-NonCommercial 4.0 International License.
Subclavian Stenosis in a Patient With Takayasu’s Arteritis and Long-Standing Ankylosing Spondylitis: Utility of IVUS Imaging
Abstract
Introduction: Takayasu’s arteritis (TA) is a chronic, idiopathic, inflammatory disease that affects large elastic arteries, including the aorta and its main branches. No consensus exists currently on the superiority of surgery over endovascular repair (angioplasty with or without stenting) for vascular lesions in TA.
Case Presentation: A 54-year-old woman with an 11-year history of ankylosing spondylitis (AS) presented with left arm weakness and severe left arm claudication. Duplex ultrasonography of the left upper extremity showed vessel-wall edema of the subclavian, axillary, and brachial arteries. Aortic angiography demonstrated a 70 - 80% stenosis of the left subclavian artery and a long, high-grade stenotic segment of the axillary artery. Intravascular ultrasound (IVUS) of the stenotic subclavian segment showed extensive negative remodeling with minimal plaque formation. The patient responded well to balloon angioplasty on this segment with medical therapy for AS.
Conclusions: Our case is the first report of IVUS imaging of subclavian stenosis resulting from Takayasu’s arteritis and provides insight into the pathology behind such lesions.
Keywords: Angiography; Other Imaging; Other treatment; Imaging
1. Introduction
Takayasu’s arteritis (TA) is a chronic, idiopathic, inflammatory disease that affects large elastic arteries, including the aorta and its main branches. When diagnosed early, it can be managed with immunosuppressive therapy and biologic agents, which can help prevent progression to steno-occlusive vascular disease. However, delayed diagnosis and disease chronicity can result in vascular lesions, with common-carotid and subclavian artery stenoses being the most common (1). No consensus exists currently on the superiority of surgery over endovascular repair (angioplasty with or without stenting) for vascular lesions in TA.
We present a case of TA involving high-grade left subclavian stenosis in the setting of long-standing ankylosing spondylitis (AS). Our patient responded to balloon angioplasty and medical therapy. Angiographic and intravascular ultrasound (IVUS) images add to our current understanding of occlusive arteriopathy in TA. Our patient is the 20th reported case of TA and AS in the English language literature.
2. Case Presentation
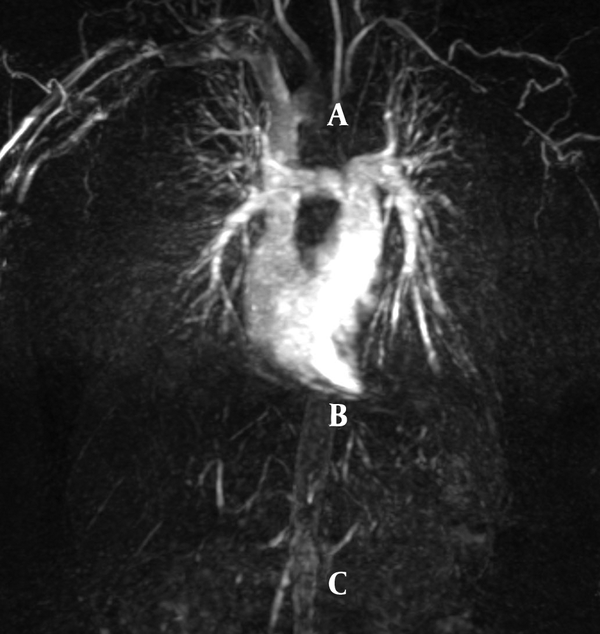
A 54-year-old woman with a history of hypertension, hyperlipidemia, Hashimoto’s thyroiditis, and HLA-B27 positive AS diagnosed 11 years previously was seen in consultation for a chief complaint of left arm weakness and severe claudication with minimal exertion. Pulses were undetectable on her left brachial and radial arteries, and her blood pressure by cuff was unobtainable. Erythrocyte sedimentation rate (ESR) was 91 mm/hour. Additional laboratory studies showed a normal C3 complement level of 160 mg/dL, a normal C4 complement level of 42 mg/dL, negative c-ANCA and p-ANCA studies, a white blood cell count of 7.16 × 103/μL, a platelet count of 228 × 109/L, and a hemoglobin of 12.3 g/dL. Duplex ultrasonography of the left upper extremity showed vessel-wall edema of the subclavian, axillary, and brachial arteries, with a wrist-brachial index of 0.79. A magnetic resonance (MR) angiogram did not demonstrate any arteritis in the thoracic and abdominal aortas, iliac arteries, and the large branch vessels of the aorta (Figure 1, MRA). She underwent coronary and aortic angiography as part of the workup, which revealed angiographically normal coronaries, but demonstrated a 70 - 80% stenosis of the left subclavian artery distal to the left internal mammary artery with post-stenotic dilatation and a long, high-grade stenotic segment of the axillary artery. This was consistent with a diagnosis of AS in accordance with the 1990 American College of Rheumatology’s (ACR’s) criteria for the classification of TA (2) as is presented in the Table 1.
|
Figure 1.
A Magnetic Resonance Angiogram Does not Demonstrate any Arteritis in the Thoracic (A) and Abdominal (B) Aortas, Iliac Arteries (C), and the Large Branch Vessels of the Aorta
|
|
Table 1.
1990 American College of Rheumatology’s Criteria for the Classification of Takayasu’s Arteritisa
|
After 2 months of persistent left upper extremity claudication symptoms associated with new-onset transient diplopia without temporal artery tenderness, the patient was started on prednisone therapy at 40 mg/d. With steroid therapy, her diplopia quickly resolved; and within 1 month, she had significant clinical improvement in her claudication symptoms, with normalization of her ESR to 9 mm/h. Repeat duplex ultrasonography of her left subclavian artery showed significant improvement, with her wrist-brachial index increased to 0.92, but with persistent smooth, long, tapered stenoses on duplex ultrasound. Over the next 6 months, she remained asymptomatic, other than weight gain associated with her steroid therapy, which was gradually tapered with adequately controlled ESR values. Prednisone was titrated further over the next 4 months. Her ESR normalized to 20 mm/h, and the wrist-brachial index was stable at 0.93. She continued to have left upper extremity claudication with minimal exertion. Surgical options for better symptoms control were discussed with her at that time, and she expressed the desire for revascularization. The options of endovascular intervention vs. long-vessel bypass grafting to the distal axillary or brachial artery were discussed, and she decided to pursue endovascular intervention.
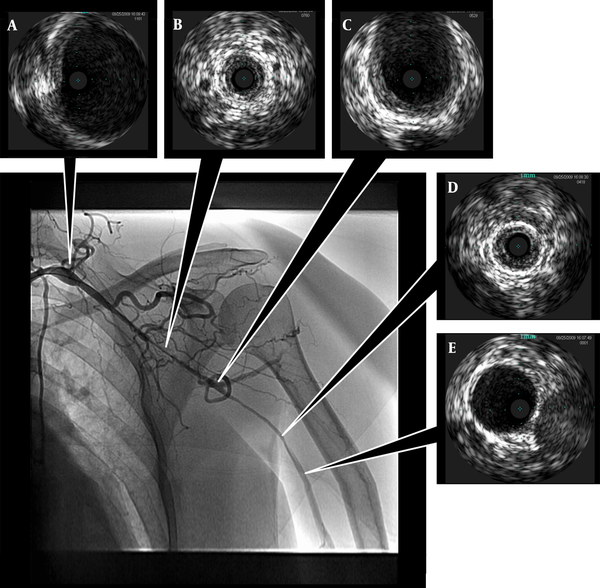
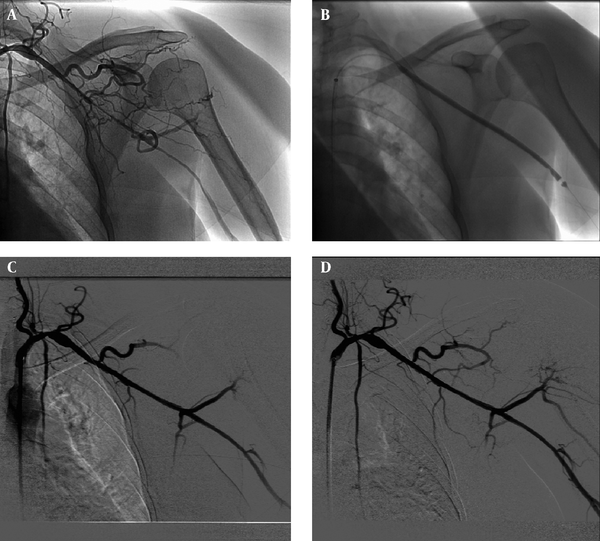
Angiography showed an initial ectatic segment of the left subclavian artery followed by high-grade (80 - 90%) 15 - 20 cm long stenotic segment extending to the left axillary artery. To better define the stenotic segments, we used intravascular ultrasound (IVUS), which showed extensive negative remodeling of the subclavian artery resulting in high-grade stenosis with only minimal plaque formation (Figure 2). At that time, her prednisone dose was stable at 15 mg/d and her ESR was 26 mm/h, consistent with the remission of the vasculitis. She was pretreated with heparin and aspirin. Under fluoroscopic guidance, a 7-F sheath was placed in the proximal left subclavian artery. A 0.014” wire was advanced to the distal left brachial artery, and balloon angioplasty was performed in an overlapping fashion with a 4 mm VascuTrakTM (Bard Peripheral Vascular, Inc, Tempe Arizona) balloon through the axillary artery to the subclavian artery in its entire length. Follow-up balloon angioplasty with a 5 × 15 VascuTrakTM balloon with repeat 4 mm high-pressure balloon angioplasty was done at a focal site of resistance. After balloon angioplasty, wide patency was achieved, confirmed by IVUS, with good angiographic flow, and a 2/2 palpable left radial pulse after the procedure (Figure 3).
|
Figure 2.
Angiogram and Intravascular Ultrasound Images
|
|
Figure 3.
Balloon Angioplasty Confers Wide Patency, Confirmed by Intravascular Ultrasound, With Good Angiographic Flow, and a 2/2 Palpable Left Radial Pulse After the Procedure
|
At follow-up 1 year later, the patient was doing well clinically without any symptoms of left upper extremity claudication. She tolerated a prednisone dose of 5 mg/d. Repeat duplex ultrasonography of the left upper extremity showed no arterial stenosis. The need to monitor her symptoms, perform surveillance studies, and continue medical therapy was emphasized.
3. Discussion
In the Table 2, we provide a summary of the previously reported cases of AS associated with TA in the English language literature. The Table also mentions the treatment done in each case.
|
Teble 2.
Summary of the Previously Reported Cases
|
The IVUS images from our case depict significant negative remodeling not apparent on angiography, with only minimal atherosclerosis causing high-grade stenosis of the left subclavian artery. As is shown in Figure 4, taking site C as the reference vessel size and site B as the tightest stenosis angiographically, there is significant shrinkage of the lumen and the external elastic membrane, which is consistent with negative remodeling. This is most likely the result of inflammation with fibrosis in the setting of long-standing AS. The patient remained symptom free at follow-up 1 year after balloon angioplasty, which indicates that although negative remodeling in the coronary vessels is associated with high rates of restenosis, (14) this might not hold true for negative remodeling in the peripheral vessels, especially if the lesion is in the setting of a long-standing inflammatory condition which is controlled appropriately post-angioplasty.
|
Figure 4.
Comparison of the highest stenosis at site; A, with the reference vessel size at site; B, shows significant shrinkage of the lumen and the external elastic membrane (EEM), which is consistent with negative remodeling; only minimal atherosclerosis is seen.
|
References
- 1. Mason JC. Takayasu arteritis: Surgical interventions. Curr Opin Rheumatol. 2015;27(1):45-52. [DOI] [PubMed]
- 2. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33(8):1129-34. [PubMed]
- 3. Paloheimo JA, Julkunen H, Siltanen P, Kajander A. Takayasu's arteritis and ankylosing spondylitis. Report of four cases. Acta Med Scand. 1966;179(1):77-85. [PubMed]
- 4. Hull RG, Asherson RA, Rennie JA. Ankylosing spondylitis and an aortic arch syndrome. Br Heart J. 1984;51(6):663-5. [PubMed]
- 5. Cowley ML, Hickling P, Wells IP, Marshall AJ. Takayasu's disease and bilateral sacroiliitis. Clin Exp Rheumatol. 1987;5(1):67-70. [PubMed]
- 6. Magaro M, Altomonte L, Mirone L, Zoli A, Corvino G. Seronegative spondarthritis associated with Takayasu's arteritis. Ann Rheum Dis. 1988;47(7):595-7. [PubMed]
- 7. Hilario MO, Terreri MT, Prismich G, Len C, Kihara EN, Goldenberg J, et al. Association of ankylosing spondylitis, Crohn's disease and Takayasu's arteritis in a child. Clin Exp Rheumatol. 1998;16(1):92-4. [PubMed]
- 8. Aoyagi S, Akashi H, Kawara T, Ishihara K, Tanaka A, Kanaya S, et al. Aortic root replacement for Takayasu arteritis associated with ulcerative colitis and ankylosing spondylitis--report of a case. Jpn Circ J. 1998;62(1):64-8. [PubMed]
- 9. Schuetz CT, Aeberli D, Oertle S, Anderson SE. Pseudoarthrosis and ankylosis of the vertebral spine without sacroiliitis associated with Takayasu's arteritis: review of the association. Skeletal Radiol. 2002;31(9):554-7. [DOI] [PubMed]
- 10. Dziadzio M, Ghattas L, Scarpelli M, Pomponio G, Gabrielli A. A case of Takayasu's arteritis with parenchymal pulmonary involvement associated with spondylarthropathy. Clin Exp Rheumatol. 2003;21(3):413-4. [PubMed]
- 11. Acar B, Yalcinkaya F, Ozturk B, Yuksel S, Ozcakar ZB, Fitoz S, et al. Seronegative spondyloarthropathy associated with Takayasu's arteritis in a child. Clin Exp Rheumatol. 2005;23(2):278-9. [PubMed]
- 12. Ben Abdelghani K, Fazaa A, Ben Abdelghani K, Laatar A, Khedher A, Zakraoui L. Chronic inflammatory rheumatism associated with Takayasu disease. Ann Vasc Surg. 2013;27(3):353 e1-6. [DOI] [PubMed]
- 13. Gan FY, Fei YY, Li MT, Wang Q, Xu D, Hou Y, et al. The characteristics of patients having ankylosing spondylitis associated with Takayasu's arteritis. Clin Rheumatol. 2014;33(3):355-8. [DOI] [PubMed]
- 14. Schoenhagen P, Ziada KM, Vince DG, Nissen SE, tuzcu EM. Arterial remodeling and coronary artery disease: the concept of "dilated" versus "obstructive" coronary atherosclerosis. J Am Coll Cardiol. 2001;38(2):297-306. [PubMed]
 Home
Home Archive
Archive Search
Search Sign In
Sign In Site Menu
Site Menu Email this article to a friend
Email this article to a friend