This Article
Citations

Except where otherwise noted, this work is licensed under Creative Commons Attribution-NonCommercial 4.0 International License.
Left Atrial Volumes and Function: Evaluation With Real-Time 3D Echocardiography in an Acute Care Setting
Abstract
Background: Limited data are available about feasibility and clinical value of left atrium (LA) quantitative evaluation obtained from real time 3D (RT-3D) echocardiography in critically ills.
Objectives: Aims of this study were: 1) to evaluate feasibility of RT-3D echocardiography for LA evaluation in an acute care setting and in a population including a majority of critically ills; 2) to evaluate correlation between two-dimensional (2D) and RT-3D echocardiographic LA quantitative evaluation; 3) to assess clinical consistency and prognostic value of LA measurements obtained from RT-3D images in subjects without CV diseases and in patients with AF and CHF, evaluated in the acute phase of the disease.
Patients and Methods: In 382 subjects admitted in the emergency department (ED), we evaluated maximal (Volmax) and minimal (Volmin) LA volumes and LA emptying fraction (LA-EF), from RT-3D images, with a semiautomated border detection program. A follow-up was performed in order to evaluate all-cause mortality and new hospital admission for cardiovascular events.
Results: The correlation between measures obtained from 2D and 3D was good (LA Volmax: r = 0.896, P < 0.001; Volmin: r = 0.906, P < 0,001; LA EF: r = 0.749, P < 0.001). Among 77 normal subjects, people aged ≥ 65 years demonstrated comparable LA dimensions with younger subjects (LA Volmax: 25 ± 11 vs 20 ± 7 mL/m2, Volmin: 11 ± 7 vs 8 ± 5 mL/m2). Subjects with normal left ventricular ejection fraction showed LA Volmax significantly lower than patients with LV systolic dysfunction or congestive heart failure (23 ± 11 vs 29 ± 10 vs 33 ± 12 mL/m2, P < 0.05). Patients in atrial fibrillation showed a significantly dilated LA compared with subjects in sinus rhytm (24 ± 11 vs 37 ± 22 mL/m2, P < 0.05). LA dimensions were significantly higher in non-survivors (LA Volmax: 33 ± 9 vs 25 ± 9 mL/m2), in patients with a new hospital admission for cardiovascular disease (LA Volmax: 34 ± 13 vs 23 ± 10 mL/m2) or with a new AF episode (LA Volmax: 40 ± 12 vs 24 ± 11 mL/m2, all P < 0.005).
Conclusions: RT-3D evaluation of LA volumes and function is feasible in a non selected series of critically ills. LA dilation was associated with a worse outcome in terms of morbidity and mortality.
Keywords: Heart Atria; Atrial Function; Echocardiography; Three-Dimensional; Critical Illness
1. Background
Enlargement of the left atrium (LA) is an independent predictors of adverse cardiovascular (CV) events in presence of a variety of cardiac disorders like atrial fibrillation (AF), congestive heart failure (CHF), coronary artery disease and cardiomyopathies (1-5). Although LA diameter has been the most widely used parameter to assess LA dimension in epidemiologic studies (3, 4, 6), it has been repeatedly demonstrated that such measure is inaccurate and yields a frequent underestimation of LA dilation (7, 8). The actually recommended measure of LA dimension is cavity volume evaluated with biplane Simpson rule or area-length formula: this is a time-consuming parameter, not easy to use in an acute-care setting (9-11).
Beyond a simple evaluation of LA dimension, LA emptying fraction (EF) and modality of atrial contribution to left ventricular (LV) filling have been preliminarily evaluated in a series of normal subjects (12) or patients affected by CHF, where they demonstrated a significant prognostic value (8, 13). A wider clinical employment of such parameters requires a feasible and accurate diagnostic tool: real time three-dimensional (RT-3D) echocardiography has been already tested in LA volume measurement and it showed an optimal diagnostic accuracy respect to a gold standard like magnetic resonance (14-16). In a critically ill patient, RT-3D echocardiography could offer the advantage of obtaining a complete data set, suitable for LV and LA quantification, from a single view; on the other hand, need for patient’s collaboration could be an important limitation (17). No data exist about RT-3D feasibility in the critically ills.
Previous papers about LA volumes and function involved exclusively selected populations of outpatients (18, 19); on the other hand, disease in which LA is heavily involved, like atrial fibrillation (AF) and congestive heart failure (CHF), are very frequent in an acute care clinical scenario (20, 21). An accurate LA evaluation could significantly improve diagnostic and prognostic stratification of patients acutely affected by these diseases.
2. Objectives
Aims of this study were: 1) to evaluate feasibility of RT-3D echocardiography for LA evaluation in an acute care setting and in a population including a majority of critically ills; 2) to evaluate correlation between two-dimensional (2D) and RT-3D echocardiographic LA quantitative evaluation; 3) to assess clinical consistency and prognostic value of LA measurements obtained from RT-3D images in subjects without CV diseases and in patients with AF and CHF, evaluated in the acute phase of the disease.
3. Patients and Methods
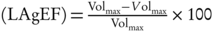
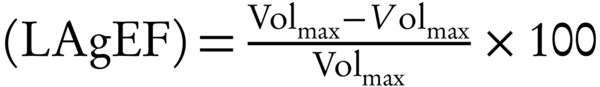
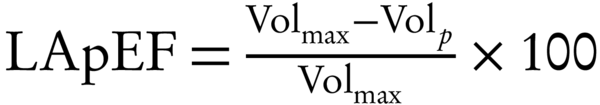
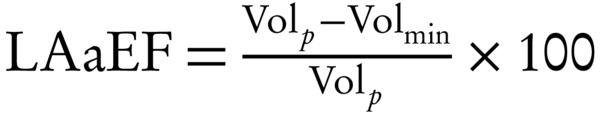
The study was conducted in the emergency department high dependency unit (ED-HDU) and in the observation unit. The ED-HDU is a sub-intensive care unit equipped with advanced monitoring, managed by emergency physicians (EP); all patients are admitted from the emergency room. Because intensive and sub-intensive care beds are limited in our reality, in the ED we created an ED-HDU where patients could be managed and stabilized for up to 48 hours, in order to reduce intensive care unit (ICU) admission. From February to September, 2011, when one of the authors (F.I.) was on-call, all echocardiographic examinations performed in the ED-HDU for standard clinical work-up, were extended to RT-3D study using a probe that allow 2D and RT-3D image acquisition (X5-1 probe, Philips Medical System). All 3D images were acquired with the specific aim to obtain the best quality images for the quantification of left atrial and ventricular cavities. In every patient we recorded the chief complaint for ED presentation, main anamnestic data and vital signs during the exam. We thus calculated modified early warning score (MEWS), that is a tool for bedside evaluation based on five physiological parameters: systolic blood pressure, pulse rate, respiratory rate, temperature and GCS score; a value ≥ 4 identifies critically ill patients (22). We did not apply any exclusion criteria according to images’ quality or admission diagnosis, in order to study an unselected population, representative of our clinical reality. Within the entire study group we classified as normal subjects those normotensive, non diabetic, in sinus rhythm, with normal LV systolic function, and without any significant cardiac valvular disease. These patients classified as normal from a cardiovascular point of view are frequently admitted for trauma and echocardiography is performed to guide fluid administration. Asymptomatic LV systolic dysfunction was defined as presence of LV ejection fraction (LV EF) < 50% in absence of any symptoms or sign of CHF, while such a diagnosis was established when typical symptoms (fatigue, effort dyspnea) and signs (pulmonary congestion, hepatomegaly, peripheral oedema) were the chief complain for admission in the ED-HDU. All patients gave their informed consent and the study is consistent with the principles of the declaration of Helsinki of clinical research involving human subjects. Transthoracic echocardiography was performed using a commercially available echocardiographic system (iE33; Philips Medical System, Andover, MA). RT-3D images were acquired by two different probes, X3-1 and X5-1: when RT-3D images were acquired using the X3-1 probe, 2D images were acquired with standard S5-1 cardiologic probe, while both 2D and RT-3D images were acquired with the same probe when X5-1 was employed. All echocardiographic images were stored digitally; LA volume measurements were systematically performed off-line with QLAB software package (QLAB 8.1, Philips Medical System, Andover, MA), by an independent reader, blinded to clinical data. RT-3D echocardiographic LA volumes were acquired in full-volume mode, from an apical window, over four cardiac cycles during quiet breathing or a breath hold. Acquisition was triggered to the electrocardiographic R wave. Care was taken to ensure that the entire LA was included within a pyramidal 3D data set. While retaining the entire left atrium within the pyramidal volume, depth and sector width were decreased as much as possible to improve the temporal and spatial resolution of the image, resulting in a volume rate of > 15 volumes/second. In patients with AF, to reduce artifacts related to variations in the cardiac cycle duration, the echocardiographic system performed an automatic check of consistency between the different sectors used to reconstruct the 3D volume and shows the real-time 3D volume on the screen to allow a final check by the operator. This process, in patients with AF, could results in a acquisition of more than 4 consecutive cardiac cycles from which the system extrapolates 4 cardiac cycles used to reconstruct the 3D volume. For each selected moment in the cardiac cycle, semiautomated tracing of LA endocardium was performed identifying 4 points in the atrial surface of the mitral annulus (anterior, inferior, lateral and septal annuli, respectively), and a fifth point at the roof of the LA. Based on these 5 points, the endocardial border was automatically traced and LA volume was obtained; manual modification was made to correct the automatic tracing if needed (Figure 1). All LA volume values were indexed for body surface area. RT 3D echocardiographic LA volumes were measured before mitral valve opening in early diastole (Volmaxi) and before mitral valve closure in end-diastole (Volmini). From this values, we evaluated LA global EF (LA gEF): In patients in SR, we measured LA volume before P wave onset on the EKG (Volpi) to derive passive (LA pEF) and active LA EF (LA aEF) as follows: 2D echocardiographic LA volumes were measured at the same times during the cardiac cycle, using bi-plane methods of disks. Endocardial border was traced manually, excluding the confluence of pulmonary veins and LA appendage. LV end-diastolic and end-systolic volumes were calculated by bi-plane methods of disks. Between July and September, 2012 all patients were contacted by telephone to verify the occurrence of new major events (death including cardiac and non-cardiac, non-fatal STEMI, new hospital admission for CHF and AF). We evaluated the following end-point: all-cause mortality, new hospital admission for CV disease and new AF episodes. Data were analyzed with SPSS program (version 19, SPSS Inc. Chicago, IL, USA). Parametric data were reported as mean ± standard deviation. The comparison between two groups was made by student’s test for non-coupled parametric data; the comparison between multiple groups was made by ANOVA test. Non parametric data were analyzed with Fisher exact test. Relations between measurements obtained from 2D and 3D were determined using Pearson’s correlation. A P value < 0.05 was considered as significant.3.1. Study Patients
3.2. Echocardiographic Data Acquisition
3.3. LA Volumes and Function by Real-Time 3D and 2D Echocardiography
(1)
(2)
(3)
3.4. Follow-Up Data
3.5. Statistical Analysis
4. Results
We retrospectively analyzed echocardiographic images of 382 subjects, mean age 67 ± 17 years, 57% male gender. The most frequent reasons for ED admission were chest pain in 40% of patients, atrial fibrillation in 12% and dyspnea in 10%. In 62 patients (16%) we were unable to derive quantitative LA volume measurements from RT 3D images: compared with patients in whom a quantitative evaluation was feasible, patients with bad image quality demonstrated a higher RR (20 ± 7 r/minute, range 11 - 45, vs 18 ± 5 r/minute, range 12 - 40, P < 0.005) and were more frequently admitted in the ED-HDU (21 vs 8%, P < 0.001) than in the Observation unit.
4.1. 2D-3D Measurements’ Correlation and Reproducibility
In a subgroup of 144 patients, we compared volumes and function evaluated by 2D and 3D echocardiography; patients in whom we evaluated 2D-3D correlations were similar to the whole study group in terms of age, LV EF, LA gEF and LA Volmaxi, Volmini and Volpi (age: 66 ± 17 vs 68 ± 17 years; LV EF: 56 ± 15 vs 53 ± 19%; LA EF: 47 ± 20 vs 44 ± 18%; LA Volmaxi 28 ± 15 vs 29 ± 14 mL/m2; LA Volmini: 16 ± 14 vs 17 ± 12 mL/m2; LA Volpi: 17 ± 8 vs 19 ± 9 mL/m2, all P = NS). The correlation was optimal for LA Volmax (4 chamber view (4C): r = 0.868; biplane evaluation (BP): r = 0.896, P < 0.001), Volmin (4C-3D: r = 0.895; BP: r = 0.906, P < 0.001) and LA EF (4C: r = 0.781; BP: r = 0.749, P < 0.001). To avoid a false high correlation driven by a single patient with a very enlarged atrium, we repeated the analysis excluding this outlier; the correlations remained very strong (LA Volmax BP-3D: r = 0.843; LA Volmin BP-3D: r = 0.860; LA gEF BP-3D: r = 0.742, all P < 0.0001).
We evaluated intra- and inter-observer reproducibility in a subgroup of 70 patients, representative of the whole study group in terms of age, LV EF, LA Volmaxi, Volmini and Volpi (age: 67 ± 18 vs 67 ± 16 years; LV EF: 53 ± 16 vs 54 ± 18 %; LA EF: 43 ± 18 vs 46 ± 19 %; Volmaxi 29 ± 13 vs 28 ± 15 mL/m2; Volmini: 18 ± 13 vs 17 ± 13 mL/m2; Volpi: 18 ± 8 vs 18 ± 9 mL/m2, all P = NS). Both intra-observer (Volmax: r = 0.936; Volmin: r = 0.941, all P < 0.0001) and inter-observer reproducibility (Volmax: r = 0.942; Volmin: r = 0.947, all P < 0.0001) were optimal.
4.2. LA Dimensions and Function in Normal Subjects
In the whole study population, we identified 77 normal subjects and we evaluated differences in LA dimensions and function according to age (62 subjects aged < 65 years vs 15 subjects aged ≥ 65 years, Table 1). LA dimensions (maximal, minimal and before P wave) were similar in both age groups; LA gEF was also similar in the two groups, while passive component of LA EF tended to be lower in older patients, in agreement with the increased contribution of LA systole to cavity emptying in this age group.
|
Table 1.
3D LA Volumes and Function According to Age in Normal Subjectsa,b,c
|
We also evaluated the correlation between age and LA dimension and function: there was a weak correlation between LA Volmaxi and age (r = 0.319, P = 0.012) and between LA Volpi and age (r = 0.467, P = 0.001), while LA Volmini and age did not exhibit any significant correlation. LA gEF did not correlate with age, while we found a mild to moderate positive correlation between age and active LA EF (r = 0.446, P = 0.001) and a moderate inverse correlation between age and LA pEF (r = −0.525, P < 0.001).
4.3. LA Dimensions and Function According to LV Function
We considered separately patients in SR (237 patients, excluding 97 patients with AF and 48 without 3D quantitative evaluation) and we divided the study population in three subgroups, respectively with normal LV function (n = 178), with asymptomatic LV systolic dysfunction (n = 40) and with symptoms of CHF (n = 19), (Table 2). At admission, patients with overt CHF were all in NYHA class III-IV; only three subjects arrived with acute pulmonary edema. The small size of this group of patients did not allow to perform a meaningful statistical analysis of LA dimensions and function according to CHF presentation.
|
Table 2.
3D LA Volumes and Function According to LV Function and Presence of CHF Signs and Symptoms (Considering Only Patients in SR)a
|
Normal subjects showed LA dimensions significantly lower than the other subgroups, with a significantly better LA gEF. LA pEF and aEF components were also higher in normal subjects, but reached a statistically significant difference only compared with patients with overt CHF.
4.4. LA Dimensions and Function According to Cardiac Rhythm
Patients with AF showed a similar 3D quantitative evaluation feasibility compared to patients in SR (80 vs 85%, P = NS).
In order to evaluate AF consequences on LA dimensions and function, we evaluated only patients with preserved LV systolic function: we identified 218 subjects, 180 in SR and 38 in AF. Patients in AF showed significantly dilated LA, with reduced LA EF (Table 3). In patients aged < 65 years, AF was not frequent in presence of a preserved LV EF and was not associated with a significant LA dilation; older patients with AF showed increased LA dimensions and a reduced LA function. Considering only subjects in SR, arterial hypertension (75 vs 37%, P < 0.0001) and diabetes (21 vs 6%, P < 0.0001) were more frequent in patients aged > 65 years, compared to younger subjects; among patients with AF prevalence of the aforementioned risk factors were similar regardless of age (hypertension: 77 vs 60%, P = NS; diabetes: 24 vs 0%, P = NS).
|
Table 3.
Patients with Normal LV Global Systolic Function: LA Dimensions and Function According to Age and Cardiac Rhythma
|
Patients with a long lasting AF demonstrated a significant LA dilation (< 48 hours, n = 18: Volmaxi 28 ± 10 mL/m2, Volmini 19 ± 10 mL/m2; > 48 hours, n = 58: Volmaxi 41 ± 20 mL/m2, Volmini 32 ± 17 mL/m2, all P < 0,05), with a significantly reduced LA function (< 48 hours: 34 ± 18%; > 48 hours: 23 ± 14%; P = 0,009) compared with patients with recent onset AF (< 48 hours).
4.5. Follow-Up
During follow-up we could contact 217 patients (57%): compared to subjects lost to follow-up, they showed similar age (66 ± 17 vs 67 ± 17 years), MEWS during the exam (1.3 ± 1.3 vs 1.4 ± 1.2) and LV EF (55 ± 18 vs 53 ± 17%, all P = NS). Twenty-six patients died, six for CV disease; 33 patients reported a new hospital admission for CV disease (most frequent diagnosis: AF in 11 patients and CHF in 6); overall 16 subjects had a new AF episode.
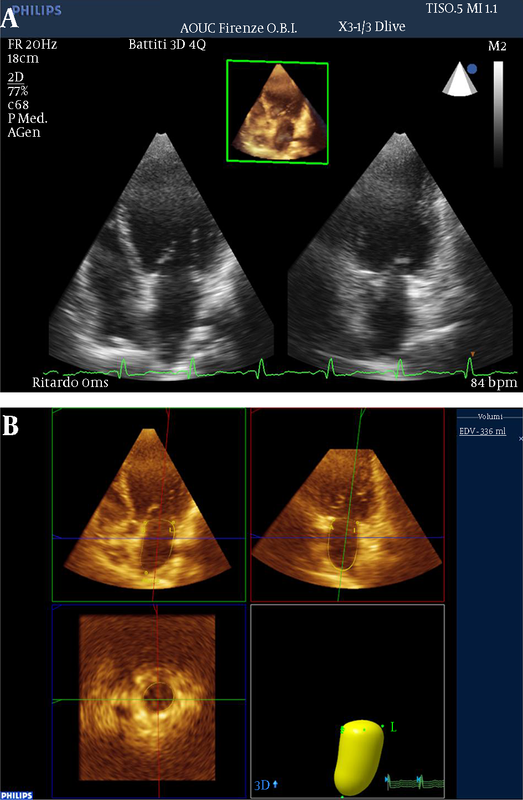
Patients who experienced each considered end-point (all cause mortality, new hospital admission for CV reason, new AF episode) exhibited significantly higher 3D LA dimensions (Figure 2A and B) and lower LA EF (Figure 2C).
|
Figure 2.
LA Maximal Volume
|
In a regression analysis adjusted for age and LV EF (Table 4) a reduced LA EF maintained an independent prognostic value for all the considered end-points; increased LA volumes were independent prognostic determinants for new hospital admission for CV disease and new AF episodes. All-cause mortality was not associated with LA volumes, a not surprising data given that a great number of patients died for non-CV disease.
|
Table 4.
LA Volumes and EF Prognostic Value in a Regression Analysis Adjusted for Age and LV EF
|
5. Discussion
In the present study, we evaluated a non selected series of patients, with a majority of subjects admitted in the ED-HDU for clinical instability and frequent vital signs alteration. In most of our patients, we could obtain good quality 3D images, that allowed us to make a quantitative evaluation of LA dimensions and function. Feasibility of a quantitative 3D evaluation implies two steps: a good quality images acquisition, that requires some degrees of patient’s collaboration, and off-line quantitative evaluation, a time-consuming process. In our study group, we could not take the first step for granted, given the high proportion of critically ills, who could give only a limited collaboration. As expected, tachypnea made 3D heart visualization significantly more difficult; however in up to 80% of patients the evaluation could be completed. From this point of view, we can say that 3D feasibility was satisfactory. To the best of our knowledge, this is the first paper in which critically ill patients were evaluated with RT-3D in order to study LA volumes and function: our results demonstrated that this technique reached a very good clinical applicability.
We observed a very good correlation between measurements derived from 2D and RT-3D images, especially for LA volumes: previous papers that evaluated this topic demonstrated a good correlation between the two measurements, with a slight underestimation by 2D in presence of LA dilation (23). For LA EF value, correlation was slightly worse compared with volume measurements: data on reproducibility of LA EF between 2D and 3D are actually lacking, so that further studies are needed to confirm our finding.
5.1. LA Volumes and Function in Normal Subjects
Among our study population we identified a small group of normal subjects: in this subgroup we could demonstrate that increasing age was not associated with any LA dilation or LA emptying deterioration. In subjects aged ≥ 65 years, we only observed a tendentially significant reduction of LA passive emptying. Correlation of LA volumes and age was very weak, while it became moderate for LA emptying passive and active fraction.
Previous papers (24, 25), both based on 2D and 3D imaging, demonstrated that physiologic aging was not associated with LA dilation. Two recent papers (26, 27) reported that only ultra-octogenarians showed significantly higher LA maximal and minimal dimensions than younger subjects; passive emptying fraction was reduced, but global and active emptying fractions were preserved. These data are in agreement with the well-known age-related reversion in E/A rate, due to reduced LV relaxation properties; however in aged subjects LA pump function is preserved, at least in part through the Starling mechanism. In fact the reduction of passive emptying increases LA dimensions at the beginning of the atrial systole and allows the maintenance of a normal active emptying and a normal contribution to overall cardiac performance.
5.2. LA Volumes and Function According to LV Function and Cardiac Rhythm
Considering only patients in SR, patients with LV systolic dysfunction and/or overt CHF showed a significant LA dilation, with reduced global emptying function; patients with an overt CHF, compared to normal subjects, demonstrated also a significant impairment of the active and passive emptying fractions. In this study population, we were not able to find significant differences between patients with asymptomatic LV dysfunction and overt CHF, probably for the small size of the group.
Considering only patients with preserved LV EF, as expected AF determined a significant LA dilation and dysfunction, that was more severe in presence of a long lasting arrhythmia. We observed that in patients aged > 65 years LA dilation was relevant, while younger subjects did not show a significant increase in atrial volume, in absence of a significant difference in comorbidities. From a prognostic point of view, we could evidence that LA RT-3D quantitative evaluation, performed in a blinded manner, gave useful clinical information, relevant for prognostic stratification: patients with a bad outcome showed significantly enlarged atrium, with a reduced emptying function. Several previous papers underlined a relevant prognostic value of LA enlargement, evaluated with 2D echocardiography, both in patients with CHF (5) and in the general population (8, 13): compared with these papers, this is the first report in which these finding are confirmed in critically ill patients evaluated with 3D echocardiography in the acute phase.
CHF is nowadays one of the main reason for patients’ presentation to the ED and represents the diagnosis with the highest short-term readmission rate: in order to identify high risk patients, new adjunctive criteria are clearly needed, beyond the well-known LV EF. A single LA volumes and function evaluation performed in the acute phase demonstrated a significant prognostic value: although these data require further evaluation in prospective studies, LA dimensions and function could become useful parameters for a prognostic stratification also in the ED clinical setting. 3D echocardiography allows to obtain complete information from a single image: therefore the adjunctive time needed for measurements is counterbalanced by a short acquisition time, that could be very useful in a critical patient. We also hope that in a near future technological improvement will further simplify measurements tools, in order to render 3D echocardiography easily applicable in a critical setting. It is plausible that the evaluation of LA dimensions and function will not modify immediate patients’ management; however, it could became very useful to improve our prognostic stratification and the ability to identify patients at higher risk of adverse prognosis.
5.3. Limitations
The retrospective design of the study allowed us to obtain a realistic picture of the kind of patients attending an ED-HDU in a real clinical scenario, but it yielded several limits and, in some cases, made subgroups non homogeneous in terms of number of cases.
An important limitation to a wider clinical applicability in an acute care setting is that RT-3D LA volumes evaluation actually requires an off-line analysis that is time-consuming, hard to be employed in a daily clinical activity. In the last few years we observed impressive improvements in 3D technology, both in image quality and in post-processing; the opportunity to employ RT-3D in critical patients was inconceivable few years ago, while we actually obtained very satisfying results. Another limitation is that we employed a semiautomated method to perform LA volumes quantitative evaluation, but we are aware that quantification tools actually available were designed to evaluate LV volumes. Anatomical differences between the two chambers could affect the accuracy of the semiautomated modality; we did not record when the manual correction was need. We wish that the recent implementation of online 3D quantification tools would represent an opportunity to reduce time for quantification systems and to make 3D a part of a routine echocardiographic exam.
5.4. Conclusions
In an unselected population including a significant proportion of critically ills, 3D images acquisition was feasible in the most part of the study population; in up to 80% of patients, we obtained quantitative evaluation of LA volumes and function. The disadvantage of being a time-consuming measure was counterbalanced by the possibility to evaluate LA volumes and function from a single image: a short acquisition time might represent a good opportunity in critically ill patients. 3D measures demonstrated a good correlation with values obtained from 2D. In normal subjects we could demonstrate that an advanced age is not associated with an LA dilation, while the passive component of atrial emptying was significantly affected by the aging process. LA dimensions and function deteriorated in presence of systolic dysfunction and in presence of AF. From a prognostic point of view, presence of LA enlargement and dysfunction was associated with a bad outcome. These data are in agreement with previous papers where 2D echocardiography was predominantly employed in an out-patients setting; with 3D echocardiography, we could confirm them in an acute care setting. Quantification tools for 3D images are actually time-consuming and require an off-line evaluation: further technical improvements are needed to make 3D really useful for daily clinical practice, also in an acute care setting.
Footnotes
References
- 1. Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. Qjm. 2001;94(10):521-6. [PubMed]
- 2. Peacock WF, Braunwald E, Abraham W, Albert N, Burnett J, Christenson R, et al. National Heart, Lung, and Blood Institute working group on emergency department management of acute heart failure: research challenges and opportunities. J Am Coll Cardiol. 2010;56(5):343-51. [DOI] [PubMed]
- 3. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):119-25. [DOI] [PubMed]
- 4. Aune E, Baekkevar M, Roislien J, Rodevand O, Otterstad JE. Normal reference ranges for left and right atrial volume indexes and ejection fractions obtained with real-time three-dimensional echocardiography. Eur J Echocardiogr. 2009;10(6):738-44. [DOI] [PubMed]
- 5. Miyasaka Y, Tsujimoto S, Maeba H, Yuasa F, Takehana K, Dote K, et al. Left atrial volume by real-time three-dimensional echocardiography: validation by 64-slice multidetector computed tomography. J Am Soc Echocardiogr. 2011;24(6):680-6. [DOI] [PubMed]
- 6. Jenkins C, Bricknell K, Marwick TH. Use of real-time three-dimensional echocardiography to measure left atrial volume: comparison with other echocardiographic techniques. J Am Soc Echocardiogr. 2005;18(9):991-7. [DOI] [PubMed]
- 7. Li F, Wang Q, Yao GH, Zhang PF, Ge ZM, Zhang M, et al. Impact of the number of image planes of real-time three-dimensional echocardiography on the accuracy of left atrial and ventricular volume measurements. Ultrasound Med Biol. 2008;34(1):40-6. [DOI] [PubMed]
- 8. Artang R, Migrino RQ, Harmann L, Bowers M, Woods TD. Left atrial volume measurement with automated border detection by 3-dimensional echocardiography: comparison with Magnetic Resonance Imaging. Cardiovasc Ultrasound. 2009;7:16. [DOI] [PubMed]
- 9. Yang HS, Bansal RC, Mookadam F, Khandheria BK, Tajik AJ, Chandrasekaran K, et al. Practical guide for three-dimensional transthoracic echocardiography using a fully sampled matrix array transducer. J Am Soc Echocardiogr. 2008;21(9):979-89. [DOI] [PubMed]
- 10. Takemoto Y, Barnes ME, Seward JB, Lester SJ, Appleton CA, Gersh BJ, et al. Usefulness of left atrial volume in predicting first congestive heart failure in patients > or = 65 years of age with well-preserved left ventricular systolic function. Am J Cardiol. 2005;96(6):832-6. [DOI] [PubMed]
- 11. Aurigemma GP, Gottdiener JS, Arnold AM, Chinali M, Hill JC, Kitzman D. Left atrial volume and geometry in healthy aging: the Cardiovascular Health Study. Circ Cardiovasc Imaging. 2009;2(4):282-9. [DOI] [PubMed]
- 12. Khoo CW, Krishnamoorthy S, Lim HS, Lip GY. Assessment of left atrial volume: a focus on echocardiographic methods and clinical implications. Clin Res Cardiol. 2011;100(2):97-105. [DOI] [PubMed]
- 13. Jiamsripong P, Honda T, Reuss CS, Hurst RT, Chaliki HP, Grill DE, et al. Three methods for evaluation of left atrial volume. Eur J Echocardiogr. 2008;9(3):351-5. [DOI] [PubMed]
- 14. Russo C, Hahn RT, Jin Z, Homma S, Sacco RL, Di Tullio MR. Comparison of echocardiographic single-plane versus biplane method in the assessment of left atrial volume and validation by real time three-dimensional echocardiography. J Am Soc Echocardiogr. 2010;23(9):954-60. [DOI] [PubMed]
- 15. Tsang TS, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, et al. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol. 2006;47(5):1018-23. [DOI] [PubMed]
- 16. Lester SJ, Ryan EW, Schiller NB, Foster E. Best method in clinical practice and in research studies to determine left atrial size. Am J Cardiol. 1999;84(7):829-32. [PubMed]
- 17. Vasan RS, Larson MG, Levy D, Evans JC, Benjamin EJ. Distribution and categorization of echocardiographic measurements in relation to reference limits: the Framingham Heart Study: formulation of a height- and sex-specific classification and its prospective validation. Circulation. 1997;96(6):1863-73. [PubMed]
- 18. Rossi A, Temporelli PL, Quintana M, Dini FL, Ghio S, Hillis GS, et al. Independent relationship of left atrial size and mortality in patients with heart failure: an individual patient meta-analysis of longitudinal data (MeRGE Heart Failure). Eur J Heart Fail. 2009;11(10):929-36. [DOI] [PubMed]
- 19. Benjamin EJ, D'Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995;92(4):835-41. [PubMed]
- 20. Bouzas-Mosquera A, Broullon FJ, Alvarez-Garcia N, Mendez E, Peteiro J, Gandara-Sambade T, et al. Left atrial size and risk for all-cause mortality and ischemic stroke. Cmaj. 2011;183(10):E657-64. [DOI] [PubMed]
- 21. Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, et al. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol. 2006;47(12):2357-63. [DOI] [PubMed]
- 22. Leung DY, Boyd A, Ng AA, Chi C, Thomas L. Echocardiographic evaluation of left atrial size and function: current understanding, pathophysiologic correlates, and prognostic implications. Am Heart J. 2008;156(6):1056-64. [DOI] [PubMed]
- 23. Anwar AM, Soliman OI, Geleijnse ML, Nemes A, Vletter WB, ten Cate FJ. Assessment of left atrial volume and function by real-time three-dimensional echocardiography. Int J Cardiol. 2008;123(2):155-61. [DOI] [PubMed]
- 24. Thomas L, Levett K, Boyd A, Leung DY, Schiller NB, Ross DL. Compensatory changes in atrial volumes with normal aging: is atrial enlargement inevitable? J Am Coll Cardiol. 2002;40(9):1630-5. [PubMed]
- 25. Pritchett AM, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM. Left atrial volume as an index of left atrial size: a population-based study. J Am Coll Cardiol. 2003;41(6):1036-43. [PubMed]
- 26. Nikitin NP, Witte KK, Thackray SD, Goodge LJ, Clark AL, Cleland JG. Effect of age and sex on left atrial morphology and function. Eur J Echocardiogr. 2003;4(1):36-42. [PubMed]
- 27. Boyd AC, Schiller NB, Leung D, Ross DL, Thomas L. Atrial dilation and altered function are mediated by age and diastolic function but not before the eighth decade. JACC Cardiovasc Imaging. 2011;4(3):234-42. [DOI] [PubMed]
 Home
Home Archive
Archive Search
Search Sign In
Sign In Site Menu
Site Menu Email this article to a friend
Email this article to a friend