This Article
Citations

Except where otherwise noted, this work is licensed under Creative Commons Attribution-NonCommercial 4.0 International License.
Carotid Artery Intima-Media Thickness in Patients Undergoing Coronary Artery Bypass Graft Surgery
Abstract
Background: Coronary artery angiography is still the gold standard of choice for detection of coronary artery disease. Nevertheless, it is an invasive procedure and its complications are not uncommon. It also predisposes patients to the potential risks of contrast study and radiation
Objective: In the present report, we aimed to assess the significance of carotid intima-media thickness (CIMT) in patients undergoing coronary artery bypass grafting (CABG) by applying an imaging approach.
Patients and Methods: The carotid arteries were evaluated at baseline with high-resolution B-mode ultrasonography by a single trained physician. Measurements were performed on the far wall of the common carotid artery in a longitudinal view. Age-adjustment was done for the measured values before deciding regarding their appropriateness in each patient. Among 215 patients undergoing CABG, 70% had a higher CIMT above the expected normal range for their ages.
Results: In our study sample, 2/3 of CAD patients requiring coronary revascularization were male. In 70% of cases carotid artery had intimal-medial thickness of above the presumed age-adjusted reference range. Traditional risk factors including hyperlipidemia, hypertension, smoking, diabetes mellitus and family history although important, but did not accurately reflect presence or extension of progression of the atherosclerotic process which could be determined by CIMT measurement. The CIMT in these patients were mostly dependent on the number and severity of the risk factors.
Conclusions: High prevalence of the increased CIMT in patients undergoing CABG highlights the significance of CIMT measurement in early diagnosis of the systemic atherosclerosis. Moreover, although Traditional cardiovascular risk factors were important they could not explain the extension and the severity of CIMT. It seems that some ultrasonographic features such as the associated carotid plaques and their characteristics provide promising clues to detect existing atherosclerosis. More importantly, avoiding the misinterpretation age-adjustment should be considered in all patients.
Keywords: Coronary Artery Bypass; Carotid Intima-media Thickness; Ultrasonography
1. Background
Coronary artery angiography is still good choice for detection of coronary artery disease. Nevertheless, it is an invasive procedure and its complications are common. It also predisposes patients to the potential risks of contrast study and radiation. More importantly, it only diagnoses coronary artery atherosclerosis in a the late stage that progression of systemic atherosclerosis has been made enough for predisposition of patients to the inevitable risks of cardio and cerebrovascular events even with highly intensive medical or revascularization interventions. On the other hand, a significant number of patients with normal epicardial coronary arteries on angiography study might be withdrawn from preventive protocols even in the presence of traditional risk factors. Moreover, as the arterial atherosclerosis is preceded be a presumably long subclinical lap phase characterized by endothelial dysfunction and gradual thickening of intima (1); early identification of atherosclerosis will be facilitated by use of modalities surrogating these early structural alterations. Consequently, in an attempt to improve cardiovascular risk stratification and enhance the preventive strategies by early diagnosis and subsequent earlier risk factor modification, a number of non-invasive, easily available, reproducible and less-expensive tools have emerged to predict the presence of systemic atherosclerosis in general population and also in high risk patients. Recently, carotid artery intima-media thickness (CIMT) is proposed to provide favorable accuracy to diagnose early atherosclerosis and have a predictive significance for myocardial infarction and stroke (2-4). When increased CIMT was detected in the common carotid segment alone, the absolute yearly risk of the event ranged from 0.7% to 2.2% for coronary heart disease (2-6), from 0.4% to 1.8% for stroke (2, 3, 5, 7, 8) and from 1.8% to 3.2% for total cardiovascular disease (5, 9). However, despite multiple scientific researches and academic papers, the clinical usefulness of this measurement has not been well accepted or adopted as a clinical tool for atherosclerosis screening in routine practice by many clinicians.
2. Objective
By applying an imaging approach, we aimed to show the diagnostic significance of CIMT in a group of patients undergoing coronary artery bypass grafting (CABG).
3. Patients and Methods
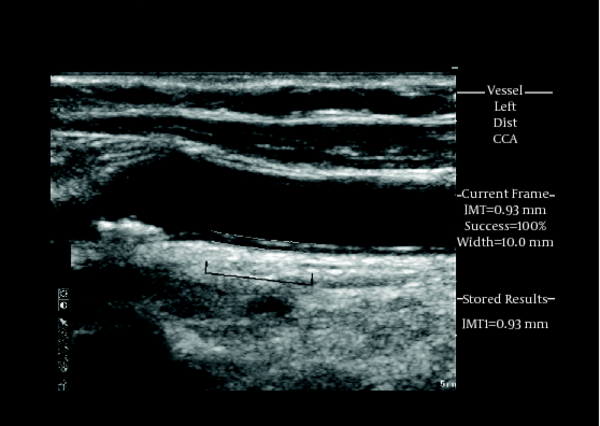
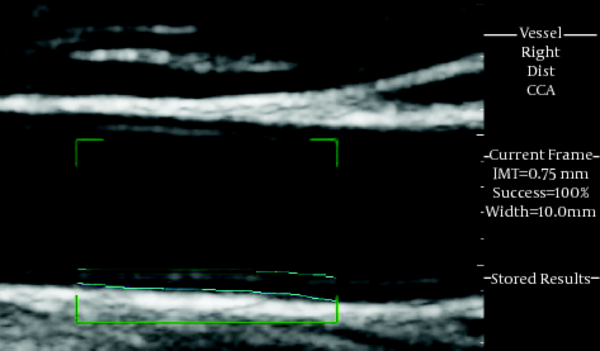
In the present report, we reviewed our single-center experience in measuring. CIMT in 215 consecutive patients, ranging 39 to 96 years of age, undergoing coronary artery revascularization from 2004 to 2012. The detailed method for the assessment of carotid artery IMT has been described in previous publications by Greedy et al. and Lucas Saba et al. (10, 11). Imaging of the very thin layer of intima requires very high frequency transducer (40 MHZ), which is only possible by intravascular ultrasound examination. Using a 10 MHZ linear transducer with wavelength of about 150 µm could not visualize the intima which measures 3-5 µm in diameter. Therefore, the ultrasound beam should be reflected from a more reflective surface like the internal elastic lamina, media and more effectively external elastic lamina which is traditionally called CIMT. The carotid arteries were evaluated at baseline with high-resolution B-mode ultrasonography. A single trained physician conducted the ultrasonographic examination and interpreted the results. For accurate measurement of CIMT, the carotid arteries should be assessed in a longitudinal view. By applying a perpendicular ultrasound beam to the artery, both near and far walls will clearly be visualized (Figure 1). This approach helps to make an accurate measurement of the arterial diameter as well. As the measurements made on the near wall depend partly on gains setting and thus are less reliable, CIMT should be measured preferably on the far wall. Furthermore, the IMT may vary along the arterial wall ; therefore, the localization of the lesion according to the end of the common carotid artery is mandatory for repositioning during the follow-up examinations. We used our previously reported normal values (SVU, June 2009), derived from patients with no traditional risk factors (Table 1), as the age-adjusted reference range (12).
|
Table1.
The age-adjusted normal values for carotid intima-media thickness (CIMT)
|
4. Results
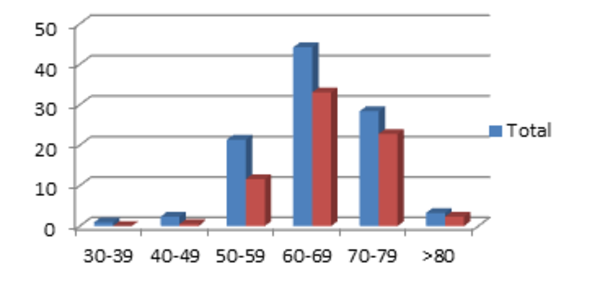
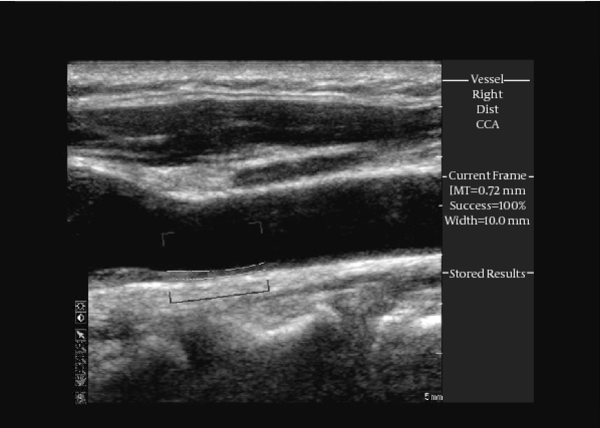
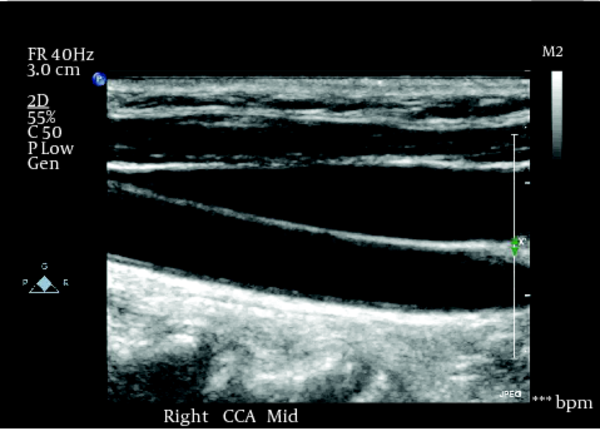
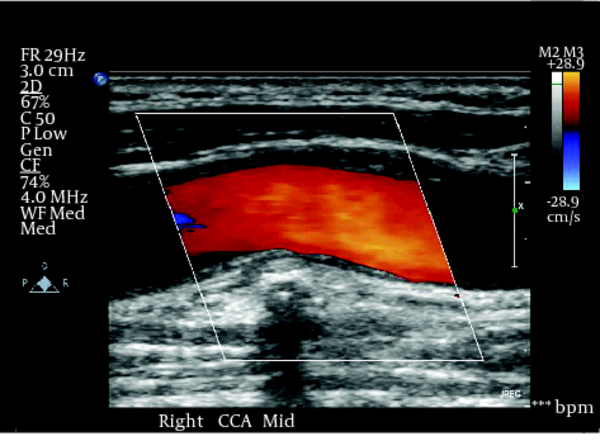
Carotid intima-media thickness was measured in 145 male (67%) and 70 female (33%) with coronary artery disease requiring coronary revascularization. The mean age of participants was 64.03 ± 12.53 years. Male and female had inconspicuous difference in CIMT (0.68 ± 0.05 versus 0.64 ± 0.04, P = 0.38). Moreover, prevalence of increased CIMT was comparable in both genders (74% in male versus 69% in female). Distribution of CIMT in various age groups is presented in Figure 2. Traditional risk factors of atherosclerosis including hyperlipidemia, hypertension, smoking, diabetes mellitus and family history of premature coronary artery disease occurred in (152) 71%, (114) 53%, (88) 41%, (158) 73% and (67) 31% of patients, respectively. In 150 (70%) of patients, carotid artery had intima-media thickness of above the presumed age-adjusted reference range. According to these age-adjusted normal values, none of the traditional risk factors were significantly different in patients with normal and increased CIMT (all P > 0.05). However, CIMT was significantly correlated with number of risk factors (r = 0.59, P = 0.007). Carotid plaques were seen in 187 (87%) of the patients and it was significantly higher in patients with increased CIMT as compared to patients with normal CIMT (83% versus 67%, P = 0.03).As shown in Figure 3, the use of color Doppler imaging may provide better visualization of atherosclerotic plaque, helping to differentiate it from CIMT.In Figure 4, CIMT is shown in a 70 year old male. A calcified atherosclerotic plaque considered distal a measurement tool.In Figure 5, double layer of a granular and heterogeneous IMT is shown in a patient with multiple CAD risk factors including smoking and hyperlipidemia.As shown in Figure 6, a CIMT of 0.72mm in a 94 year old male is considered better than expected for his age. Despite a relatively high incidence of CIMT in CAD patients undergoing CABG, the presence of CAD cannot be predicted by the CIMT alone.
|
Figure 1.
As shown here, by applying a perpendicular ultrasound beam to the artery both near and far walls will clearly be visualized
|
|
Figure 2.
Distribution of Increased Carotid-Intima Media Thickness (CIMT) in Various Age Groups
|
|
Figure3.
Color Doppler makes the IMT and plaque visualization more revealing. Double layers of a heterogeneous IMT are shown from a patient with multiple risk factors for CAD.
|
|
Figure 4.
CIMT in association with a calcified plaque in a 70 year old male with CAD. The presence of plaque increases the diagnostic significance of CIMT.
|
|
Figure 5.
Sonolucent media with granular pattern is shown in a CAD patient with dyslipidemia and current smoking.
|
|
Figure 6.
A CIMT of 0.72mm is shown in a 90 year old male, which is considered better than expected for his age.
|
5. Discussion
It has been shown that the increase in CIMT may function as a surrogate marker with a very high correlation with an increased risk of cardio- and cerebro-vascular diseases. Our results demonstrated that although traditional risk factors including hyperlipidemia, hypertension, smoking, diabetes mellitus and family history of premature CAD were important, they did not accurately reflect the presence or extension of progression of atherosclerotic process which could be determined by CIMT measurement. The CIMT in these patients were mostly dependent on the number of the risk factors. To avoid possible misleading, two major lesions of carotid arteries, the plaques and the CIMT, should be differentiated carefully. On ultrasound examination, CIMT is seen as a double-line pattern on both walls of the CCAs in a longitudinal image. It consists of two parallel lines, which are the leading edges of two anatomical boundaries including the lumen- intima and media-adventitia interfaces, While the Plaque is a protuberating focal lesion into the arterial lumen, measuring at least 0.5 mm or 50% of the adjacent IMT value, or demonstrating a thickness of more than 1.5 mm as measured from the media-adventitia interface to the intima-lumen interface (13). It was shown previously that carotid total plaque presence (14, 15) or plaque area is more closely linked to the coronary artery disease, and have higher predictive value of coronary events (3, 16-18), compared to CIMT. Moreover, it is now recognized that different ultrasonographic features of arterial atherosclerosis including CIMT, plaque area and stenosis have different biological (19-21) and genetic (22) basis. As shown previously, traditional coronary risk factors present only 15% to 17% cases with increased CIMT (23, 24), while carotid total plaque area correlates with the presence of traditional risk factors in 52% of patients (25). This may suggest the higher association of carotid plaque area with atherosclerosis than CIMT (26). In the present study, we emphasized the significance of associated lesions pointing to the presence of atherosclerotic process. Interestingly, the presence of concomitant atherosclerotic plaques significantly enhances the predictive value of the CIMT measurement (27). Moreover, the characteristics of such plaques such as central sonolucency and thin cap, but less for the plaque calcifications, would carry an important additional value for identifying the clinically relevant CIMT (7, 28). Similar to the plaques, the CIMT describing characteristics such as softness, homo-or heterogeneity and smoothness or irregular surface are probably as significant as the CIMT in making decisions regarding the diagnostic significance of this lesion. However, the question whether which CIMT patterns might raise the clinical significance of CIMT, first noted by our study, needs to be addressed in future investigations to provide sufficient evidence. In the present report we also highlighted the age-normalization for CIMT. Atherosclerosis is a progressive process and its association with aging is inevitable. The appropriate interpretation of the results based on the potential confounding factors such as age, gender, race, the presence of associated cardiovascular risk factors and even the co-morbid conditions seem to be more important than judgment on the CIMT value alone (29-32). For example, a CIMT of 0.45mm in a 39 year old male or a CIMT of 0.52mm in a 41 year old male may be considered age-appropriate while a CIMT of 0.55mm in a 69 year old male or CIMT of 0.59 mm a 75 year old male is considered better than expected for their age. Moreover, a CIMT of 0.70mm in a 59 year old male is inappropriately thick. In our opinion, this technic is still a research tool rather than a definite predictive measure of the cardiovascular diseases. Associated cardiovascular risk factors, concomitant carotid plaques, age-adjustments or probably the characteristics of the CIMT may provide useful clues to a systemic atherosclerotic process.
Acknowledgments
There is nothing no acknowledge.
Footnotes
References
- 1. Ross R. Atherosclerosis: current understanding of mechanisms and future strategies in therapy. Transplant Proc. 1993;25(2):2041-3. [PubMed]
- 2. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96(5):1432-7. [PubMed]
- 3. O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK, Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340(1):14-22. [DOI] [PubMed]
- 4. Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11(5):1245-9. [PubMed]
- 5. Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke. 2006;37(1):87-92. [DOI] [PubMed]
- 6. Rosvall M, Janzon L, Berglund G, Engstrom G, Hedblad B. Incident coronary events and case fatality in relation to common carotid intima-media thickness. J Intern Med. 2005;257(5):430-7. [DOI] [PubMed]
- 7. Kitamura A, Iso H, Imano H, Ohira T, Okada T, Sato S, et al. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004;35(12):2788-94. [DOI] [PubMed]
- 8. Rosvall M, Janzon L, Berglund G, Engstrom G, Hedblad B. Incidence of stroke is related to carotid IMT even in the absence of plaque. Atherosclerosis. 2005;179(2):325-31. [DOI] [PubMed]
- 9. Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2008;168(12):1333-9. [DOI] [PubMed]
- 10. Loizou CP, Pattichis CS, Nicolaides AN, Pantziaris M. Manual and automated media and intima thickness measurements of the common carotid artery. IEEE Trans Ultrason Ferroelectr Freq Control. 2009;56(5):983-94. [DOI] [PubMed]
- 11. Saba L, Tallapally N, Gao H, Molinari F, Anzidei M, Piga M, et al. Semiautomated and automated algorithms for analysis of the carotid artery wall on computed tomography and sonography: a correlation study. J Ultrasound Med. 2013;32(4):665-74. [PubMed]
- 12. Alipour M,, Doan HA, Bean B. Normal values of Intima-Media Thickness (IMT) in patients with no traditional Risk Factors (RF) for Atherosclerosis. Society of Vascular Ultrasound 2009 Annual Conference; 2009.
- 13. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34(4):290-6. [DOI] [PubMed]
- 14. Ebrahim S, Papacosta O, Whincup P, Wannamethee G, Walker M, Nicolaides AN, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: the British Regional Heart Study. Stroke. 1999;30(4):841-50. [PubMed]
- 15. Prati P, Tosetto A, Vanuzzo D, Bader G, Casaroli M, Canciani L, et al. Carotid intima media thickness and plaques can predict the occurrence of ischemic cerebrovascular events. Stroke. 2008;39(9):2470-6. [DOI] [PubMed]
- 16. Chan SY, Mancini GB, Kuramoto L, Schulzer M, Frohlich J, Ignaszewski A. The prognostic importance of endothelial dysfunction and carotid atheroma burden in patients with coronary artery disease. J Am Coll Cardiol. 2003;42(6):1037-43. [PubMed]
- 17. Johnsen SH, Mathiesen EB, Joakimsen O, Stensland E, Wilsgaard T, Lochen ML, et al. Carotid atherosclerosis is a stronger predictor of myocardial infarction in women than in men: a 6-year follow-up study of 6226 persons: the Tromso Study. Stroke. 2007;38(11):2873-80. [DOI] [PubMed]
- 18. Spence JD, Eliasziw M, DiCicco M, Hackam DG, Galil R, Lohmann T. Carotid plaque area: a tool for targeting and evaluating vascular preventive therapy. Stroke. 2002;33(12):2916-22. [PubMed]
- 19. Spence JD, Hegele RA. Noninvasive phenotypes of atherosclerosis: similar windows but different views. Stroke. 2004;35(3):649-53. [DOI] [PubMed]
- 20. Spence JD, Hegele RA. Noninvasive phenotypes of atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24(11):ee188 author reply e188-9 [DOI] [PubMed]
- 21. Spence JD, Hegele RA. Non-invasive assessment of atherosclerosis risk. Curr Drug Targets Cardiovasc Haematol Disord. 2004;4(2):125-8. [PubMed]
- 22. Pollex RL, Hegele R. Genetic determinants of carotid ultrasound traits. Curr Atheroscler Rep. 2006;8(3):206-15. [PubMed]
- 23. Al-Shali K, House AA, Hanley AJ, Khan HM, Harris SB, Mamakeesick M, et al. Differences between carotid wall morphological phenotypes measured by ultrasound in one, two and three dimensions. Atherosclerosis. 2005;178(2):319-25. [DOI] [PubMed]
- 24. O'Leary DH, Polak JF, Kronmal RA, Savage PJ, Borhani NO, Kittner SJ, et al. Thickening of the carotid wall. A marker for atherosclerosis in the elderly? Cardiovascular Health Study Collaborative Research Group. Stroke. 1996;27(2):224-31. [PubMed]
- 25. Spence JD, Barnett PA, Bulman DE, Hegele RA. An approach to ascertain probands with a non-traditional risk factor for carotid atherosclerosis. Atherosclerosis. 1999;144(2):429-34. [PubMed]
- 26. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. 2010;30(2):177-81. [DOI] [PubMed]
- 27. Suurkula M, Agewall S, Fagerberg B, Wendelhag I, Widgren B, Wikstrand J. Ultrasound evaluation of atherosclerotic manifestations in the carotid artery in high-risk hypertensive patients. Risk Intervention Study (RIS) Group. Arterioscler Thromb. 1994;14(8):1297-304. [PubMed]
- 28. Polak JF, Shemanski L, O'Leary DH, Lefkowitz D, Price TR, Savage PJ, et al. Hypoechoic plaque at US of the carotid artery: an independent risk factor for incident stroke in adults aged 65 years or older. Cardiovascular Health Study. Radiology. 1998;208(3):649-54. [PubMed]
- 29. Jourdan C, Wühl E, Litwin Mi, Fahr K, Trelewicz J, Jobs K, et al. Normative values for intima-media thickness and distensibility of large arteries in healthy adolescents. Journal of Hypertension. 2005;23(9):1707-15.
- 30. Litwin M, Trelewicz J, Wawer Z, Antoniewicz J, Wierzbicka A, Rajszys P, et al. Intima-media thickness and arterial elasticity in hypertensive children: controlled study. Pediatr Nephrol. 2004;19(7):767-74. [DOI] [PubMed]
- 31. Urbina EM, Srinivasan SR, Tang R, Bond MG, Kieltyka L, Berenson GS. Impact of multiple coronary risk factors on the intima-media thickness of different segments of carotid artery in healthy young adults (The Bogalusa Heart Study). Am J Cardiol. 2002;90(9):953-58.
- 32. Yang XZ, Liu Y, Mi J, Tang CS, Du JB. Pre-clinical atherosclerosis evaluated by carotid artery intima-media thickness and the risk factors in children. Chin Med J (Engl). 2007;120(5):359-62. [PubMed]
 Home
Home Archive
Archive Search
Search Sign In
Sign In Site Menu
Site Menu Email this article to a friend
Email this article to a friend