This Article
Citations

Except where otherwise noted, this work is licensed under Creative Commons Attribution-NonCommercial 4.0 International License.
Cerebrovascular Accident and Mesenteric Ischemia Following Diagnostic Coronary Angiography
Abstract
Introduction: Coronary angiography can be complicated by some major complications such as stroke.
Case Presentation: We describe a patient who presented with hemiparesia. He had undergone coronary angiography on his right and left coronary arteries as well as his left ventricle (LV) via the radial artery access 10 days earlier using a 6-French Tiger catheter. Transthoracic echocardiography showed a large (36 × 25 mm) inhomogeneous mobile mass attached to the apicoseptal LV segment. His serum protein S was low (60% [normal = 77 - 140%]), while his protein C was normal and lupus anticoagulant was negative. During hospitalization, he developed severe abdominal pain, for which mesenteric ischemia was diagnosed. First, he underwent surgery for the resection of the infarcted intestinal segments. Then cardiac surgery was done to remove the mass. The mass was diagnosed as a thrombus. After the surgery, the general condition of the patient deteriorated and blood culture showed acinetobacter septicemia. Finally, he died due to sepsis. A review of his coronary angiography revealed that after the contrast media had left the LV, there was still dye at the contact point between the tip of the catheter and the LV, which was compatible with the location of thrombus formation.
Conclusions: Trauma induced by the tip of the catheter at the contact location with the LV wall in a patient with mild hypercoagulable state accounted for intracardiac thrombosis formation and its embolization to the brain and intestines.
Keywords: Angiography; Thrombosis; Stroke; Ischemia
1. Introduction
Coronary artery angiography is an established diagnostic method to visualize coronary arteries. It yields valuable information about the anatomy of coronary arteries and is required in many ischemic heart disease patients before planning further treatments. However, this invasive method may be associated with major or minor complications. Major complications reported include death, myocardial infarction, and stroke (1). Local vascular complications include arteriovenous fistula, pseudoaneurysm, and arterial thrombosis (1). Here, we present our experience with a patient who developed complications following coronary angiography via the radial artery access, which has been reported to have a lower rate of complications than the femoral artery access.
2. Case Presentation
A 49-year-old patient was brought to our hospital after awakening at midnight and noticing inability to talk and move his right-sided extremities. Brain computed tomography (CT) was performed, which showed ischemic lesion. The vital signs were within the normal range. Heart, lung, and abdomen examinations were unremarkable. Neurologic examination revealed muscle strength of 4/5 on the right side and 5/5 on the left side. He had Broca’s aphasia. The left lower extremity was cold, and the pulses were not detectable. Electrocardiography was normal. The patient was admitted for further evaluations. He did not have diabetes mellitus, dyslipidemia, or hypertension. Past history revealed that he had had limp, pain, and cold extremities in the past 6 months for which CT angiography had been done. On CT angiography, there were significant stenotic lesions bilaterally in the iliac and femoral arteries with predominance on the left side. Hence, he was candidated for aortofemoral bypass surgery. Ten days earlier, coronary artery angiography on his right and left coronary arteries as well as his left ventricle (LV) via the radial artery access using a 6-French Tiger catheter had been done for him in another medical center which was reported as normal as well as transthoracic echocardiography (TTE) which was unremarkable. It is likely that coronary angiography had been done in order to exclude the possibility of simultaneous coronary artery disease with regard to the diagnosis of peripheral vascular disease which had been made for the patient.
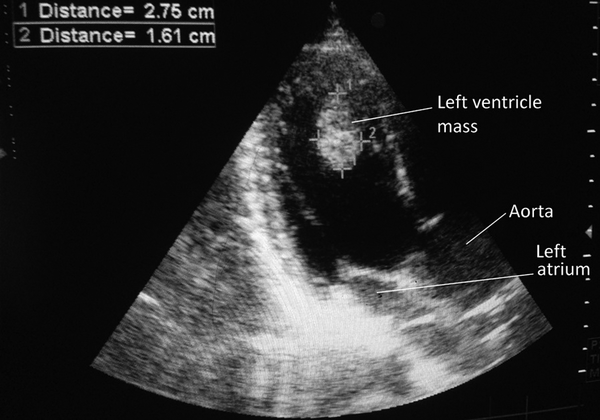
Laboratory data showed leukocytosis (WBC = 21,700/mm3, neutrophil = 90%, lymphocyte = 2%, and eosinophil = 1%), normal hemoglobin (14.5 gr/dL), and thrombocytosis (platelet count = 608,000/mm3), but normal PT, PTT, and INR. Electrolytes were normal. Inflammatory markers were increased (ESR = 49 mm/hour and CRP = 123 mg/dL). On TTE, the LV size and function were normal (ejection fraction = 55%), but there was a large (36 × 25 mm) inhomogeneous mobile mass attached to the apicoseptal LV segment (Figure 1). There was mild tricuspid regurgitation as well as mitral regurgitation. The right ventricular (RV) size and function were normal (Videos 1 and 2). The patient was started on a therapeutic dose of IV unfractionated heparin and consultations with rheumatology and cardiac surgery services were asked. Further rheumatologic laboratory results were normal except for a low protein S of 60% (normal = 77-140%). Protein C was normal, and lupus anticoagulant was negative. During hospitalization, the clinical course of the patient deteriorated and he developed visual blurring and right upper extremity paresis. He also developed acute-onset severe periumbilical abdominal pain and hematochezia. His abdominal pain aggravated rapidly, and he developed abdominal general tenderness. With the presumed diagnosis of mesenteric ischemia, he underwent emergency laparotomy and intestinal resection (two-thirds of the small intestine and total colectomy) was done. After stabilization, he underwent cardiac surgery (middle sternotomy) and the cardiac mass was removed. On gross examination during the cardiac surgery, the mass was pinkish and fragile with weak attachment to the LV apical wall. After cardiac surgery, the patient developed fever and low consciousness. Brain CT scan did not show any new abnormal findings except for the ischemic lesion which had been observed on the first brain CT image; consequently, the possibility of a new ischemic stroke was remote. Repeated TTE did not reveal any pathology, which rendered the possibility of another thrombus formation unlikely. We, therefore, focused on his fever and performed sepsis work-up. Blood culture showed acinetobacter. Despite receiving wide spectrum IV antibiotics, the patient died due to sepsis. Histopathological examination of the cardiac mass reported it as thrombosis. Since there was no abnormal LV wall motion, the video of his coronary angiography was reviewed. Angiography had been done via the radial artery using a 6-French Tiger catheter. The coronary arteries were patent. There was no filling defect. It was noticed that after the contrast media had left the LV, there was still dye at the contact point between the tip of the catheter and the LV, which was compatible with the location of thrombus formation.
|
Figure 1.
Transthoracic Echocardiography (TTE), Showing a Large Inhomogeneous Mobile Mass Attached to the Apico-Septal Left Ventricular Segment
|
3. Discussion
Having reviewed all aspects of the events happening to our patient, we concluded that most probably trauma induced by the incidental contact between the tip of the catheter and the LV endothelium caused thrombosis formation at the LV wall. Consequently, after 10 days, embolization of this intracardiac thrombosis presented itself first in the form of stroke (hemiparesia and Broca’s aphasia). Embolization to the brain occurred once more, and he experienced neurologic signs when hospitalized. And for the third time, embolization caused mesenteric ischemia. We speculate that thrombosis formation probably occurred due to some mild form of hypercoagulable state detected in this patient as demonstrated by his low protein S level. Intracardiac thrombus formation is a rare complication during angiography. Generally, local vascular complications occur less frequently with the radial artery access and even radial access is associated with better outcomes (2, 3). Nevertheless, there is no information on other major complications in this arterial access way. Mesenteric ischemia has been reported previously as a complication, though very rare, of coronary angiography (4, 5). The interesting point here that differs from the previous reports is that mesenteric ischemia, noted by previous reports, did not happen during or shortly after angiography. Compared to mesenteric ischemia, stroke (ischemic or hemorrhagic) is a more known complication of coronary angiography. Most authors have reported factors such as debris or cholesterol particles which dislodge and cause stroke (6). However, our patient’s angiography did not show coronary artery calcifications. In conclusion, coronary angiography is an invaluable diagnostic instrument in mapping the anatomy of the coronary arteries. However, this modality can be associated with some complications. Here we noted some rare simultaneous complications (ischemic stroke and mesenteric ischemia) as a cause of intracardiac thrombus formation. We, accordingly, recommend that cardiologists exercise due caution regarding the LV contrast injection and select the best catheter available as well as the best possible place in order to lessen the likelihood of complications.
Acknowledgments
We thank the radiology and laboratory services of Shariati Hospital for their support.
Footnotes
References
- 1. West R, Ellis G, Brooks N, Joint Audit Committee of the British Cardiac S, Royal College of Physicians of L. Complications of diagnostic cardiac catheterisation: results from a confidential inquiry into cardiac catheter complications. Heart. 2006;92(6):810-4. [DOI] [PubMed]
- 2. Greenwood MJ, Della-Siega AJ, Fretz EB, Kinloch D, Klinke P, Mildenberger R, et al. Vascular communications of the hand in patients being considered for transradial coronary angiography: is the Allen's test accurate? J Am Coll Cardiol. 2005;46(11):2013-7. [DOI] [PubMed]
- 3. Sciahbasi A, Pristipino C, Ambrosio G, Sperduti I, Scabbia EV, Greco C, et al. Arterial access-site-related outcomes of patients undergoing invasive coronary procedures for acute coronary syndromes (from the ComPaRison of Early Invasive and Conservative Treatment in Patients With Non-ST-ElevatiOn Acute Coronary Syndromes [PRESTO-ACS] Vascular Substudy). Am J Cardiol. 2009;103(6):796-800. [DOI] [PubMed]
- 4. Ibis C, Sezer A, Coskun I. A very rare complication of coronary angiography: Acute mesenteric ischemia. Ind J Surg. 2006;68(3):171-2.
- 5. ter Woorst FJ, Berry LL, de Swart HJ, van Ommen VA, Prenger KB. A rare complication of coronary arteriography. Cathet Cardiovasc Diagn. 1998;43(4):455-6.
- 6. Eggebrecht H, Oldenburg O, Dirsch O, Haude M, Baumgart D, Welge D, et al. Potential embolization by atherosclerotic debris dislodged from aortic wall during cardiac catheterization:: Histological and clinical findings in 7,621 patients. Cathet Cardiovasc Diagn. 2000;49(4):389.
 Home
Home Archive
Archive Search
Search Sign In
Sign In Site Menu
Site Menu Email this article to a friend
Email this article to a friend